WHAT IS MAST CELL ACTIVATION SYNDROME (MCAS)? THE IMMUNE SYSTEM GONE ROGUE
Mast Cell Activation Syndrome (MCAS) represents a condition where the body's mast cells—important components of the immune system—release excessive amounts of chemicals inappropriately. These cells are meant to help your body fight infections and heal wounds, but in MCAS, they become hyperreactive, releasing their contents (called mediators) without appropriate triggers or in excessive amounts. This disorder can affect multiple systems throughout the body, leading to a wide range of symptoms that can vary greatly in severity.
MCAS has gained increased recognition in recent years, though many patients still face challenges in diagnosis due to its complex presentation and overlap with other conditions. As research advances, the medical community continues to develop a better understanding of this challenging disorder that affects quality of life for many individuals.
Causes and Risk Factors
The exact cause of Mast Cell Activation Syndrome remains under investigation, but researchers have identified several potential contributors:
Genetic Factors: Certain genetic mutations may influence how mast cells are regulated in some individuals. Some patients have been found to carry variations in the KIT gene, which encodes a protein essential for mast cell development.
Environmental Triggers: For many with MCAS, exposure to certain triggers can set off reactions.
Common triggers include:
Specific foods or food additives
Medications (especially NSAIDs, opioids, and antibiotics)
Insect stings or bites
Temperature extremes
Physical stress
Emotional stress
Hormonal changes
Infections
Environmental chemicals and fragrances
Associated Conditions: MCAS appears to occur more frequently in people with certain other conditions, suggesting potential connections:
Ehlers-Danlos Syndrome (a connective tissue disorder)
Postural Orthostatic Tachycardia Syndrome (POTS)
Autoimmune disorders
Irritable Bowel Syndrome (IBS)
Fibromyalgia
Research suggests that prior infections, injuries, or prolonged stress may play a role in triggering the initial dysfunction in mast cells, though the exact mechanisms remain unclear.
Common Symptoms
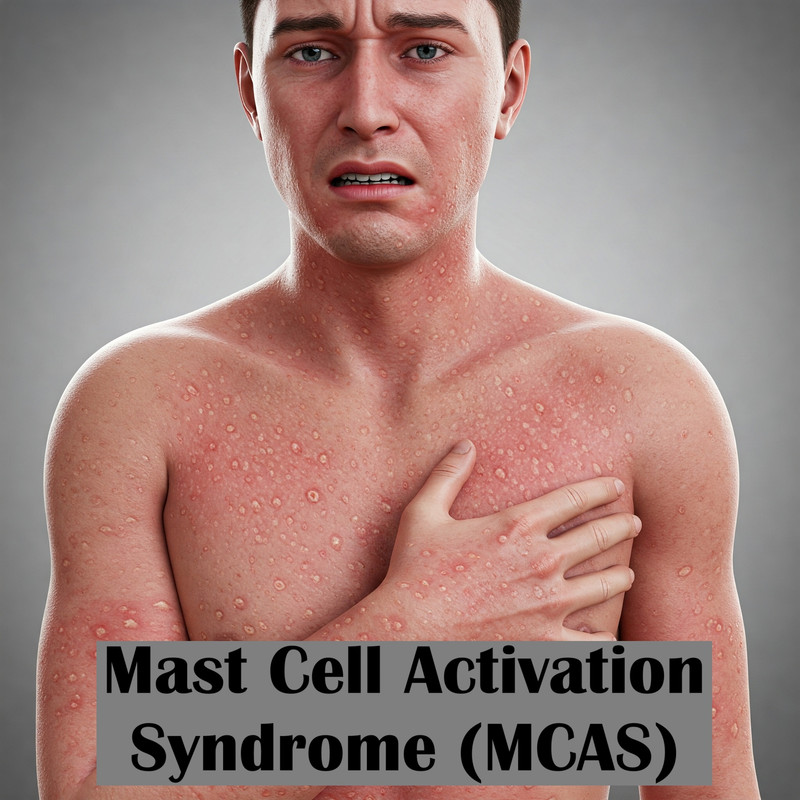
MCAS can affect virtually any system in the body, which explains why symptoms can be so varied and wide-ranging. Common manifestations include:
Skin Symptoms:
Flushing or redness
Hives or rashes that come and go
Itching
Gastrointestinal Symptoms:
Abdominal pain
Diarrhea and/or constipation
Nausea and vomiting
Heartburn
Bloating
Cardiovascular Symptoms:
Rapid heart rate (tachycardia)
Blood pressure changes
Lightheadedness or fainting
Respiratory Symptoms:
Wheezing
Shortness of breath
Throat tightness
Congestion
Neurological Symptoms:
Headaches
Brain fog or difficulty concentrating
Memory issues
Anxiety
Insomnia
The hallmark of MCAS is the fluctuating nature of symptoms—they may come and go, vary in intensity, and affect different body systems at different times. This variability often leads to diagnostic challenges and can be extremely frustrating for patients.
Diagnosis Methods
Due to its complexity, diagnosing Mast Cell Activation Syndrome (MCAS) requires a thorough and multidisciplinary approach.
Medical History: A detailed history is crucial, particularly noting symptom patterns, potential triggers, and response to medications.
Laboratory Tests:
Serum tryptase levels (preferably during and between reactions)
24-hour urine tests may be used to measure mediators such as N-methylhistamine and prostaglandin D2.
Serum histamine levels
Chromogranin A
Challenge Testing: In some cases, controlled exposure to suspected triggers may be performed in a medical setting.
Medication Response: Improvement with medications that target mast cell mediators can support diagnosis.
Exclusion of Other Conditions: Since many symptoms overlap with other disorders, ruling out alternative explanations is essential.
Diagnosis is particularly challenging because:
1. Mast cell mediators are unstable and may degrade before testing
2. Symptoms fluctuate and laboratory abnormalities may not be present during testing
3. There's no single definitive test
Many patients benefit from seeing specialists familiar with mast cell disorders, such as allergists/immunologists, hematologists, or specialists in mast cell diseases.
Treatment Options
Treatment for MCAS typically follows a multimodal approach:
Medications:
1. H1 Antihistamines (like cetirizine, loratadine): Help control itching, hives, and allergic symptoms
2. H2 Antihistamines (like famotidine, ranitidine): Address gastrointestinal symptoms and work with H1 blockers
3. Mast Cell Stabilizers, including cromolyn sodium and ketotifen, help inhibit the release of inflammatory substances from mast cells.
4. Leukotriene Inhibitors (like montelukast): Can help with respiratory symptoms
5. Corticosteroids: Used short-term for severe flares
6. Aspirin: In some cases, under medical supervision (though NSAIDs typically worsen symptoms in many MCAS patients)
Lifestyle Modifications:
1. Trigger Avoidance: Identifying and avoiding personal triggers
2. Anti-inflammatory Diet: Many patients benefit from eliminating common trigger foods
3. Stress Management: Techniques like meditation, deep breathing, and gentle exercise
4. Temperature Regulation: Avoiding temperature extremes
5. Consistent Sleep Schedule: Maintaining regular sleep patterns
Supportive Therapies:
Physical therapy to maintain function
Psychological support to cope with chronic illness
Nutritional guidance to ensure adequate nutrition despite dietary restrictions
Treatment plans are highly individualized, and finding the right combination often requires patience and close collaboration with healthcare providers.
Prevention and Management Tips
While MCAS cannot be completely prevented, these strategies may help manage symptoms and reduce flare-ups:
Keep a Symptom Journal: Track potential triggers, symptoms, and their timing
Develop an Emergency Plan: Work with your doctor to create a plan for severe reactions
Wear Medical ID: Consider wearing medical identification if you experience severe reactions
Practice Good Sleep Hygiene: Prioritize quality sleep
Stay Hydrated: Adequate hydration supports overall health and may help flush mediators
Introduce Changes Gradually: Whether new foods, medications, or activities, make changes one at a time to monitor responses
Build a Support Network: Connect with family, friends, or support groups who understand chronic illness
Practice Gentle Movement: Low-impact exercise like walking, swimming, or gentle yoga when tolerated
When to See a Doctor
Seek medical attention if you experience:
Recurrent episodes of symptoms affecting multiple body systems without clear explanation
Symptoms that significantly impact your quality of life
Severe allergic-type reactions, especially those involving breathing difficulties or significant drop in blood pressure
Persistent gastrointestinal issues alongside skin or respiratory symptoms
Symptoms that don't respond to typical treatments for allergies or other conditions
If MCAS is suspected, it’s advisable to consult an allergist or immunologist experienced in mast cell disorders. Bring a detailed record of your symptoms, their triggers, and timeline to appointments.


Comments
Post a Comment